
Introduction
Delayed graft function (DGF) is a common complication of kidney transplantation that can negatively impact short- and long-term outcomes. However, the extent of its adverse impact on transplant outcomes remains unclear. A systematic review and meta-analysis of studies published between 2007 and 2020 were conducted to investigate the association between DGF and post-transplant outcomes. The analysis revealed that DGF was associated with increased odds of graft failure, acute rejection, and mortality. These findings could inform the selection process, treatment, and monitoring of transplanted kidneys at high risk of DGF. The study also looked at the effects of DCD (donation after cardiac death) status on DGF outcomes and highlighted the increasing utilization of less-than-ideal organs for transplantation. Despite the increasing incidence of DGF, improvements in short- and long-term outcomes for allografts have been observed. This raises questions about the changing relationship between DGF incidence and post-transplant outcomes. Overall, this meta-analysis underscores the importance of identifying and managing DGF early to improve transplant outcomes.
Materials & Methods
This article describes the methods used for a systematic review of studies investigating the associations between delayed graft function (DGF) and kidney transplant outcomes. The review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 guideline, and the search strategy included PubMed and Embase databases, as well as scoping searches in other databases. The inclusion criteria were studies published in English between January 2007 and March 2020, with a primary aim of investigating the effect of DGF on transplant outcomes and including at least one outcome of interest (graft survival, acute rejection, patient mortality, kidney function). Data were independently extracted from the included studies by two researchers, and statistical analysis of the outcomes was performed using STATA 17.0. Subgroup analysis was performed to investigate differences in outcomes between donation after brain death (DBD) and donation after circulatory death (DCD) kidneys. Publication bias was assessed using funnel plots and the Egger test of asymmetry, and risk of biases in individual studies were conducted using the Cochrane risk of bias tool.
Results
The searches from Pubmed and Embase yielded 1512 and 1910 studies, respectively, with 1128 of the articles being duplicates between the 2 databases. A total of 2087 studies were excluded after title and abstract review in which post transplant outcomes of DGF were not included in the study. Full text of the remaining 207 studies were assessed, and 156 studies were subsequently excluded, which resulted in 51 studies that met the inclusion criteria. Among these 51 articles, 5 more studies were excluded because they included overlapping cohorts, and an additional 8 studies were excluded because of raw data unavilability. As a result, a total of 38 studies were included for detailed review, data extraction, and analysis (Figure 1).

Graft Failure
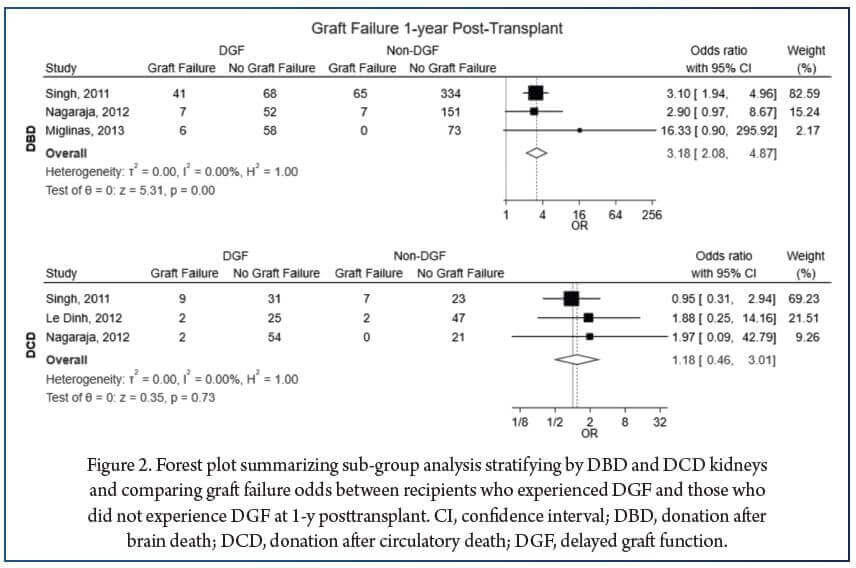
This study analyzed 38 studies on graft failure outcomes in patients who experienced delayed graft function (DGF) after transplantation. 29 studies compared DGF patients to non-DGF patients, with 23 being single-center studies and 6 registry-based. Patients who experienced DGF had significantly higher odds of graft failure compared to those who did not experience DGF at 1-, 3-, and 5-years post-transplant in both single-center and registry-based studies. The odds of graft failure were higher in DBD kidney transplants but not in DCD transplants (Figure 2).
Acute Rejection
About 58% of the 38 studies included in the analysis reported on the incidence of acute rejection in patients with or without DGF after kidney transplantation. Among the 19 single-center studies and three registry- based studies, DGF was found to be significantly associated with higher odds of acute rejection at 1- and 3-year post-transplantation. The effect was similar for registry-based studies.
Patient Mortality
About 58% of the 38 studies investigated the association between DGF and patient mortality. Of these, 18 were single-center studies and 4 were registry-based studies. Patients who experienced DGF had higher odds of mortality than those who did not at 1-y post-transplant and 5-y post-transplant in single-center studies. However, no significant increase in the odds of mortality at 3-y post-transplant was observed. In registry-based studies, patients who experienced DGF had significantly higher odds of mortality at 3-y post-transplant.
Kidney Function
The variability in how kidney function was measured in the studies limited the ability to aggregate data. Only eGFR levels at 1-year post-transplant were analyzed from 11 single-center studies, which reported eGFR levels as calculated using different formulas. On average, individuals who experienced DGF had a lower eGFR by 5.46 mL/min/1.73 m2 compared to those who did not experience DGF at 1-year post-transplant.
Discussion
Delayed graft function (DGF) is a common complication of kidney transplantation. DGF has been shown to be associated with significantly worse short- and long-term outcomes post-transplant, including increased graft failure, acute allograft rejection, and mortality. The causes for the attenuation of DGF with longer-term adverse outcomes are yet to be elucidated, but may stem from an overall improvement in post-transplant outcomes over the years. To better understand the differential effect of DGF on graft outcomes, more studies need to stratify their analysis between donation after brain death (DBD) and donation after cardiac death (DCD) kidneys. There is a compelling need for a more informative and standardized definition of DGF. Improved understanding of the impact of DGF on longer-term posttransplant outcomes will help centers be more accepting of kidneys that are perceived to be associated with a higher risk of DGF for transplantation to recipients in dire need.
References:
1. Yarlagadda SG, Coca SG, Formica RN Jr, et al. Association between delayed graft function and allograft and patient survival: a systematic review and meta-analysis. Nephrol Dial Transplant. 2009;24:1039–1047.
2. Zeraati AA, Naghibi M, Kianoush S, et al. Impact of slow and delayed graft function on kidney graft survival between various subgroups among renal transplant patients. Transplant Proc. 2009;41:2777–2780.
3. Singh RP, Farney AC, Rogers J, et al. Kidney transplantation from donation after cardiac death donors: lack of impact of delayed graft function on post-transplant outcomes. Clin Transplant. 2011;25:255–264.
4. Jayaram D, Kommareddi M, Sung RS, et al. Delayed graft function requiring more than one-time dialysis treatment is associated with inferior clinical outcomes. Clin Transplant. 2012;26:E536–E543.
5. Salazar Meira F, Zemiacki J, Figueiredo AE, et al. Factors associated with delayed graft function and their influence on outcomes of kidney transplantation. Transplant Proc. 2016;48:2267–2271.
6. Helfer MS, Pompeo JC, Costa ORS, et al. Long-term effects of delayed graft function duration on function and survival of deceased donor kidney transplants. J Bras Nefrol. 2019;41:231–241.
7. Heilman RL, Smith ML, Smith BH, et al. Progression of interstitial fibrosis during the first year after deceased donor kidney transplantation among patients with and without delayed graft function. Clin J Am Soc Nephrol. 2016;11:2225–2232.
8. Lim WH, McDonald SP, Russ GR, et al. Association between delayed graft function and graft loss in donation after cardiac death kidney transplants-a paired kidney registry analysis. Transplantation. 2017;101:1139–1143.
9. Tapiawala SN, Tinckam KJ, Cardella CJ, et al. Delayed graft function and the risk for death with a functioning graft . J Am Soc Nephrol. 2010;21:153–161.
10. Figueiredo A, Moreira P, Parada B, et al. Risk factors for delayed renal graft function and their impact on renal transplantation outcome. Transplant Proc. 2007;39:2473–2475.
11. Premasathian N, Avihingsanon Y, Ingsathit A, et al. Risk factors and outcome of delayed graft function after cadaveric kidney transplantation: a report from the Thai Transplant Registry. Transplant Proc. 2010;42:4017–4020.
12. Augliene R, Dalinkeviciene E, Kuzminskis V, et al. Factors influencing renal graft survival: 7-year experience of a single center. Medicina (Kaunas). 2017;53:224–232.
13. Gavela Martínez E, Pallardó Mateu LM, Sancho Calabuig A, et al. Delayed graft function after renal transplantation: an unresolved problem. Transplant Proc. 2011;43:2171–2173.
14. Lai Q, Pretagostini R, Poli L, et al. Delayed graft function decreases early and intermediate graft outcomes after expanded criteria donor kidney transplants. Transplant Proc. 2009;41:1145–1148.
15. Gill J, Dong J, Rose C, et al. The risk of allograft failure and the survival benefit of kidney transplantation are complicated by delayed graft function. Kidney Int. 2016;89:1331–1336.
16. Coemans M, Süsal C, Döhler B, et al. Analyses of the short- and long-term graft survival after kidney transplantation in Europe between 1986 and 2015. Kidney Int. 2018;94:964–973.
17. Gopalakrishnan G, Gourabathini SP. Marginal kidney donor. Indian J Urol. 2007;23:286–293.
18. Miglinas M, Supranaviciene L, Mateikaite K, et al. Delayed graft function: risk factors and the effects of early function and graft survival. Transplant Proc. 2013;45:1363–1367.




